Pustulosis Palmaris et Plantaris (PPP)
What is Pustulosis palmaris et plantaris?


Pustulosis palmaris et plantaris (PPP) is a rare and chronic pustular and inflammatory condition whose exact cause is still not fully understood. It primarily affects the palms of the hands and soles of the feet.
It is also called Palmoplantar Pustulosis. Palmoplantar (Palmo meaning palm, plantar meaning sole) pustulosis is a persistent (chronic) condition that causes blisters filled with fluid on the palms and the soles of the feet.
Is Palmoplantar Pustulosis a form of psoriasis?
Some dermatologists have proposed that PPP is a variant of psoriasis. Therefore, its treatment is similar to psoriasis. However, this topic is still controversial.
The signs and symptoms of Palmoplantar Pustulosis include itchy and painful skin of the palms or soles, especially if there are deep cracks in the skin (fissures).
Although PPP is not cancerous or contagious, the inflammation of the palms and soles can severely affect one’s quality of life. It can be painful and itchy, making it hard for one to walk or use their hands – possibly affecting sleep, work, and activities of daily living. There are, however, several treatments for Palmoplantar Pustulosis that can improve it significantly. The most crucial step is to stop smoking or never start.
The ordinary dermatologists prescribe strong steriodal oinments such as Dermovate (clobetasol propionate ), Diflal (diflorasone diacetate),or Diacort (diflorasone diacetate). Steroid creams and ointments reduce inflammation in the skin. Unfortunately, the skin can get used to steroids, so that they may have less benefit if applied continuously. But, since the skin of the limbs is thick, you do not have to worry about side effects such as skin thinning caused by steroids, even if you apply a potent steroidal lotion. Whatever the degree of potency for steroidal ointments for Palmoplantar Pustulosis, the condition is often not improved.
Dermatologists may also recommend oral prescription of vitamin A derivatives. Some suggest surgeries like a tonsillectomy or appendix excision. However, despite these efforts, the treatment is not remarkably effective enough to cure the symptoms.
The most effective treatment method for Palmoplantar Pustulosis
There are different treatment options for Palmoplantar Pustulosis ranging from creams to phototherapy to tablets. The treatment approaches are specific to the patients depending on the severity of their condition. The protocol of the treatment at my clinic is quite different from treatments in common clinics. And from my practices, I can assure you that you will be free from Palmoplantar Pustulosis in almost a year by following my treatment protocol. The success rate of my protocol is more than 90% as long as you abstain from smoking and sleep early by 10 pm.
I have described my treatment procedure briefly here as:
1) Amoxycillin
For the first week, take Amoxycillin. But if you are allergic to penicillin, please avoid it.
As PPP is said to be aseptic, the use of antibiotics can be pointless. Even so, if you take antibiotics, especially Amoxycillin, at an early stage, your condition can improve promptly.
2) Erythromycin / Cepharanthine
From the second week, take Erythromycin (Erythrocin®) and Cepharanthine (Cepharanthin®).
Erythromycin ( Erythrocin® 200 mg )
Erythromycin is an antibiotic used in the treatment and prevention of several bacterial infections. Theoretically, antibiotics are only effective against bacteria, but realistically, Erythromycin seems to be effective against the virus as well. Therefore, I recommend this as good medicine for Palmoplantar Pustulosis. As for myself, whenever I travel overseas on long flights, I always take Erythromycin as prophylactic for two days before the flight. It works for the prevention of both bacterial and viral infections.
As PPP is aseptic theoretically, we are not quite sure why Erythromycin is an effective medicine. But in the medical field, actual disease is very different from theory.
(https://en.wikipedia.org/wiki/Erythromycin)
(https://en.wikipedia.org/wiki/Cepharanthine)
How to take: 4 tablets/day — Morning (2 tablets) and Evening (2 tablets). But the process of taking is unique. Please take the medication as follows:
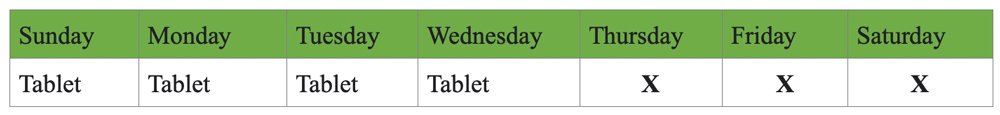
As shown above, take the 4 tablets for four days and don’t take them for the following three days. For example, if you begin from Sunday, take 4 tablets/ day for Monday, Tuesday, Wednesday. And on Thursday, Friday, Saturday, you should discontinue the medication. You should again continue the same pattern by taking 4 tablets every day from the next Sunday to Wednesday and keeping a gap from Thursday to Saturday.
Repeat this cycle for 12 weeks (almost 3 months).
*If you are allergic to Macrolides, please don’t take this antibiotic.
Cepharanthine ( Cepharanthin® 1 mg )
It is a naturally occurring alkaloid extracted from the plant Stephania cepharantha Hayata. In Japan, Cepharanthin® is a somewhat obscure medicine. As it is inexpensive, doctors are not interested in prescribing it (Doctors prefer costly drugs for business!!), and Cepharanthine is often underrated. Despite its value, it helps to cure diseases like Multiple Sclerosis, Ulcerative Colitis, and Hypothyroidism. Being able to modulate the immune system, Cepharanthin is beneficial in the cure of Palmoplantar Pustulosis.
Now, only one Japanese company manufactures Cepharanthin. I do hope the other companies continue the production of this notably potent PPP pill.
How to take: 3 to 4 tablets/day. Generally, you must continue it for 3 months.
It has few side effects in contrast to biologics such as Stelara or immunosuppressants such as MTX.
3) Ointment PS(1)
With more than 15 years of research, analysis, and completion, and treatment of more than 40,000 patients with varieties of skin diseases, we have created a unique formula – PS (1) for the cure of PPP. You should apply PS(1) every day on the lesion twice a day till the lesion gets healed completely. The components of PS(1) are:
Difluprednate, clofibrate, jojoba oil, vegetable squalene, lanolin hydrous, macadamia nut oil, fermented extract of leaves of shell ginger, very fine powder of 5 kinds of mineral ores.
4) Supplements for Palmoplantar Pustulosis
With the medicine and ointments, the symptoms get cured in 3 to 4 months. Even if the symptoms are relieved, you should take a few supplements to maintain the therapy for one or two years. These supplements are effective not only for PPP but also for general health:
- Shell Ginger (JIPANG Ginger®) (2 to 4 capsules/day)
- Biotin (10,000 mcg – 15,000 mcg/day)
- α-Lipoic Acid (600 mg – 1,000 mg/day)
- Harp Seal Oil (3,000 mg/day)
- Inositol (500 mg – 1,000 mg/day)
- Probiotic
a) Shell Ginger (JIPANG Ginger®)
Skin is the largest detoxification organ of the body. Thus, detoxification is a must whether you have atopic dermatitis, psoriasis, PPP, or other skin problems.
One of the outstanding benefits of Shell Ginger is detoxification. Shell Ginger improves bowel movement, which aids in the release of harmful substances in the body. However, in most cases, temporary symptoms can develop for about a week to a month. It can cause discomfort in patients but, there is no need to worry. After the deterioration time is over, the recovery time improves impressively.
You can take 2 to 4 capsules/day. However, if the temporary aggravation is severe, please reduce it to 1 capsule/day or 1 capsule/every alternate day. You can read more information about the Shell Ginger supplement on the page of https://makiselifeup.com/product/jipang-ginger/
b) Biotin
Biotin (a kind of vitamin B-complex) falls among the essential vitamins. In Palmoplantar pustulosis treatment, biotin is very effective. This vitamin is required for fat metabolism and thus influences skin health.
Patients using antibiotics, intaking only α-lipoic acid, following dialysis, and consuming an excessive amount of egg white are likely to be deficient in this vitamin. Besides, people taking sleeping pills, antidepressants, and antiepileptic drugs for a longer duration also lack biotin. As some species of lactic acid bacteria feed on biotin, you must limit intake of yogurt cautiously.
Dosage of biotin for Palmoplantar Pustulosis: 10 mg to 15 mg/day. Please do not mistake the unit. It is 10 mg to 15 mg (10,000 mcg to 15,000 mcg), not 10 mcg to 15 mcg (10 μg to 15 μg). Many biotin supplements contain 5000 mcg of biotin per capsule. Hence, the recommendation is 2-3 capsules per day in such cases.
You should continue biotin supplements for at least six months. Please avoid smoking, as biotin does not work efficiently with smoking
c) α-Lipoic Acid
α-Lipoic acid is an antioxidant, both soluble in water and lipid. Due to this property, α-Lipoic acid helps to recycle Vitamin C and Glutathione (water-soluble antioxidants), Vitamin E, and CoQ 10 (fat-soluble antioxidants). In simple terms, α-Lipoic acid increases the efficiency of antioxidants. With the intake of the α-lipoic acid supplement, the level of glutathione is increased by 30%.
α-Lipoic acid also reduces CoQ 10 (which recycles vitamin E). Studies have confirmed that α-Lipoic acid compensates for its deficiency even if Vitamin E is deficient for some reason.
d) Harp Seal Oil (3,000 mg)
Harp seal oil is one of the best supplements for Palmoplantar Pustulosis as it plays a vital role in reducing inflammation. It is very stable, contains EPA, DHA, and DPA, and is the best source of omega-3 fatty acids. These essential fatty acids circulate in human blood and maintain soft, plaque-free arterial walls. They also reduce inflammation and produce a healing effect on the cells of the skin. Furthermore, from these unsaturated fatty acids, beneficial eicosanoids are metabolized. It facilitates the cure of PPP.
But, if you love such a cute animal as Harp Seal and would not like to sacrifice their lives, you can choose Sacha Inchi Oil. And if you would like to economize, Flaxseed Oil or Perilla Oil can be a good substitute for omega-3 fatty acids.
e) Inositol
Inositol is a vitamin-like substance synthesized in small quantities in our bodies. Phytate, naturally present in cereals and grains, acts as a precursor of inositol. Phytin, phytic acid, and inositol have different functions, such as maintaining cholesterol levels and promoting skin health. It can improve disorders in the nervous system such as neuropathy caused by diabetes, panic syndrome, and obsessive-compulsive disorder. Besides, it can alleviate Polycystic ovary syndrome (PCOS).
Concerning the skin, Inositol relates to the dermal stem cells in the dermis. This dermal stem cell enhances dermis regeneration and repairability and maintains youthful skin. For this, there should be stabilization of dermal stem cells around blood vessels.
Platelet-Derived Growth Factor (PDGF) helps in the regeneration of dermal stem cells. Inositol promotes the expression of the gene of growth factor and maintains skin health.
f) Probiotics
Probiotics improve digestion by increasing good bacterias and crowding out harmful bacterias in our gut. Please read more about probiotics here>>
5) Avoid Iron Supplement.
You should not take any unnecessary iron supplements unless you are diagnosed with iron deficiency anemia. There is an association between the metabolism of iron and Palmoplantar Pustulosis. When anemic patients with PPP take iron supplements, their condition deteriorates, as red blood cells contain iron.
Excess iron aggravates various kinds of skin diseases. It explains why blood donation is often effective in curing skin problems and why the symptoms ease when a PPP patient gets phlebotomy (bloodletting).
Please don’t take excess vitamin C supplements, as it stimulates the absorption of iron. So, please avoid foods rich in iron, such as prune and spinach. However, you can eat fruits and vegetables rich in Vitamin C.
Some tips for maintaining a good diet and lifestyle for Palmoplantar Pustulosis
Though it might not be possible to prevent all cases of Palmoplantar Pustulosis, here are some tips for maintaining the treatment:
- If you smoke, try to stop. The cause is unclear, but there’s a known link between Palmoplantar Pustulosis and smoking. Nicotine in tobacco products can affect your skin cells and cause inflammation in your sweat glands, especially on your hands and feet. Thus, if you stop smoking, your symptoms may get better.
- Wear 100% cotton socks, and choose comfortable footwear made from natural fibers.
- Avoid friction and minor injuries. Any injuries, even minor ones, can be troublesome on your skin. If you have an injury, use waterproof bandages.
- Rest the affected areas and keep them clean.
Protect your skin. Wear gloves when you work with water, use household cleaners, or do manual labor. - Moisturize your skin. Use moisturizing creams and ointments on your palms and soles.
- Don’t use a bubble bath or shower gel. Replace them with moisturizing cleaning products for the skin.
- If you have recurrent tonsillitis, consult the doctor if surgery is possible.
- Use salicylic acid or urea creams on the feet to reduce skin thickening and dead skin.
- Follow a strict gluten-free diet if you have coeliac disease.
- Go to bed early and sleep at least for 7 hours a day. The growth hormone secretes from the pituitary gland between 11 pm to 3 am (3 hours after you fall asleep). For this reason, you must go to bed at least by 11 pm – the best is 9 or 10 pm. Similarly, when the blood glucose level is high, the pituitary gland cannot secrete growth hormones sufficiently. Thus, do not go to bed at least 2 hours after dinner.
Although there is no definite cure for Pustulosis palmaris et plantaris, various measures are adopted to manage symptoms. Always remember that PPP can be subjective, so choose a suitable lifestyle, diet, and medication.
Copyright: No reproduction or republication without written permission.
